Scoliosis is a complex spinal condition characterized by 3D structural changes in the spine and trunk. It manifests as a lateral curvature of the spine, measured on X-ray using a Cobb angle of 10 degrees or more, along with rotational abnormalities (1, 2, 3).
Various factors, including congenital and neuromuscular conditions, can contribute to the development of scoliosis. When the underlying cause of scoliosis cannot be identified, it is classified as idiopathic scoliosis. When this condition occurs in individuals aged 10-18 years, it is referred to as adolescent idiopathic scoliosis (AIS) (3).

AIS affects approximately 5% of the adolescent population, with the most significant progression of the deformity occurring during the rapid growth phase of puberty. Consequently, early diagnosis and prompt provision of treatment options are crucial for optimal patient outcomes (3, 4, 10).
A Common Issue: Missed Diagnosis
Regrettably, there is substantial evidence suggesting that the diagnosis of AIS is frequently missed, resulting in an average delay of approximately 14 +/- 9 months (5). All healthcare professionals have a vital role to play in ensuring that these children are not overlooked. Recognizing the subtle signs, symptoms, and red flags associated with scoliosis enables early intervention through treatment or referral to specialized professionals (5).
The Importance of Early Diagnosis for Teens
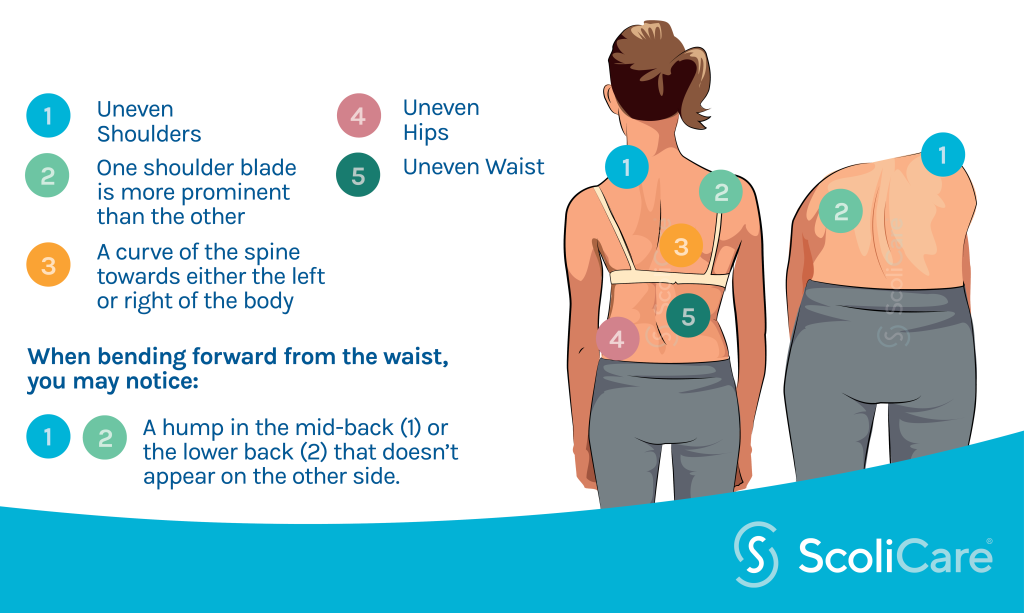
Why is early diagnosis particularly crucial for adolescents with scoliosis? Delayed diagnosis allows the condition more time to progress. As the spinal curves become more pronounced, there is progressive deformity of the vertebrae and discs, leading to asymmetry in the trunk. Observable changes include waist and rib cage asymmetry, uneven shoulder and scapulae positions (Figure 2). Early diagnosis provides patients with more opportunities to prevent curve progression through the implementation of conservative treatment options, such as scoliosis-specific exercise programs (e.g., ScoliBalance®), and, for larger curves, a custom-made 3D rigid brace (e.g., ScoliBrace®).
Identifying Scoliosis in Adolescents
Healthcare professionals are well-positioned to screen and identify potential cases of scoliosis in adolescents.
Typically, once an adolescent has completed their growth, the likelihood of curve progression decreases. However, this is mostly applicable if the curve remains below a Cobb angle measurement of 30 degrees on X-ray (3). Adolescents who complete their growth phase with curves exceeding 30-50 degrees are at higher risk of progression and other associated problems later in life (3).
It’s important to note that the longer the diagnosis is delayed, the greater the risk of curve progression and the development of deformities.
Recognizing Signs and Symptoms of Scoliosis
In AIS, trunk rotation resulting from spinal rotation leads to trunk asymmetry. This can be observed during the Adam’s Forward Bend Test (Figure 2), where one side of the trunk appears more elevated than the other (1, 2). The extent of rotation and asymmetry can be measured using a small device called a Scoliometer, which quantifies the Angle of Trunk Rotation (ATR) (6).
A positive result on the Adam’s Forward Bend test should prompt a referral to a suitably trained healthcare professional for further evaluation. Indications for X-ray may include an ATR reading of 5 degrees in the lumbar region and 7 degrees in the thoracic region. However, it is important to note that these figures may inadvertently miss some cases. Referring patients with lower ATR values may be necessary due to the following reasons:
- Rotation and deformity can occur at smaller ATR measurements.
- A pelvic obliquity caused by sacral deformity or leg length discrepancy can mask a lumbar scoliosis. These figures were primarily used in large-scale adolescent screenings, such as in school settings, to minimize unnecessary X-rays. However, in one-on-one scenarios with patients, where a more comprehensive assessment is possible, it is easier to identify individuals who require referral. A diagnosis of scoliosis is confirmed when a patient has a Cobb angle of 10 degrees or more on X-ray, accompanied by rotation (Figure 4). AIS is diagnosed when the patient is between 10 and 18 years old, and no known cause for the scoliosis has been identified (7).
Treatment Options for Scoliosis
Current international guidelines strongly recommend early treatment for AIS (3). This includes physiotherapeutic scoliosis-specific exercises (PSSE) for curves up to approximately 20-25 degrees, and PSSE combined with bracing for larger curves (3).
Once the curves progress beyond approximately 45 degrees, adolescents are often referred for surgical consultation. While there may not be a medical urgency for surgery at this point, research suggests that curves reaching this threshold are more likely to progress into adulthood (7). Conversely, emerging evidence supports conservative treatment options for individuals who opt not to undergo surgery, even with curves at the surgical level (8).
How to Avoid Missing an AIS Diagnosis

As healthcare professionals, it is imperative that each of us plays a role in advocating for early diagnosis in children with scoliosis. Once a diagnosis is made and treatment options are provided, the subsequent course of action becomes the decision of the patient and their family. However, this process cannot occur if cases are overlooked. By following a few simple steps, you can contribute to the prevention of progression in these patients and help ensure they receive timely care.
Tips for Recognizing Scoliosis:
- Promote the use of self-screening at home. One option is the ScoliCare app, developed specifically for this purpose (https://app.scoliscreen.com).
- Familiarize yourself with the signs and symptoms that may indicate the presence of AIS. These can include uneven shoulders, asymmetrical waist angles, scapulae positioning, rib prominence, spinal curvature, and a positive Adam’s Forward Bend Test.
- Recognize that some patients with AIS may experience pain, while others may not (9). The absence of pain should not deter you from referring a patient for further evaluation.
- Be aware of local resources and professionals to whom you can refer patients. ScoliCare has clinics across Australia and the USA, and there are ScoliBrace® Providers and ScoliBalance® Providers worldwide.
Remember, early diagnosis offers patients a wider range of options for management and better long-term outcomes. By remaining vigilant and proactive, we can make a significant difference in the lives of adolescents with scoliosis.
References
- Dunn J, Henrikson NB, Morrison CC, Blasi PR, Nguyen M, Lin JS. Screening for adolescent idiopathic scoliosis: evidence report and systematic review for the US preventive services task force. Jama. 2018;319(2):173-87.
- Grossman DC, Curry SJ, Owens DK, Barry MJ, Davidson KW, Doubeni CA, et al. Screening for adolescent idiopathic scoliosis: US preventive services task force recommendation statement. Jama. 2018;319(2):165-72.
- Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis and spinal disorders. 2018;13(1):1-48.
- Bunnell WP. An objective criterion for scoliosis screening. JBJS. 1984;66(9):1381-7.
- Kenner P, McGrath S, Woodland P. What factors influence delayed referral to spinal surgeon in adolescent idiopathic scoliosis? Spine. 2019;44(22):1578-84.
- Krawczyński A, Kotwicki T, Szulc A, Samborski W. Clinical and radiological assessment of vertebral rotation in idiopathic scoliosis. Ortopedia, Traumatologia, Rehabilitacja. 2006;8(6):602-7.
- Choudhry MN, Ahmad Z, Verma R. Adolescent idiopathic scoliosis. The open orthopaedics journal. 2016;10:143.
- Rigo M, Reiter C, Weiss H-R. Effect of conservative management on the prevalence of surgery in patients with adolescent idiopathic scoliosis. Pediatric rehabilitation. 2003;6(3-4):209-14.
- Théroux J, Le May S, Fortin C, Labelle H. Prevalence and management of back pain in adolescent idiopathic scoliosis patients: a retrospective study. Pain Research and Management. 2015;20(3):153-7.
- Konieczny MR, Senyurt H, Krauspe R. Epidemiology of adolescent idiopathic scoliosis. Journal of Children’s Orthopaedics. 2013;7(1):3-9. doi:10.1007/s11832-012-0457-4
